Taking care of moms
CMU’s AI and human decision-making researchers create an app to improve maternal mortality.
Tamar Krishnamurti worries about the alarming rates of preterm birth and maternal mortality in the United States, particularly for black mothers.
“There’s no good reason women of color are dying at four times the rate of other women from pregnancy complications,” Krishnamurti said. So, she applied her expertise in behavioral science to do something about it.
Krishnamurti holds a courtesy position in Carnegie Mellon University’s department of Engineering and Public Policy (EPP) as well as an assistant professorship of medicine and clinical and translational science at the University of Pittsburgh.
She and her colleague Alex Davis, assistant professor of EPP, have been collaborating since they were in graduate school together at CMU, combining his machine learning expertise with her behavioral and decision science insights.
Krishnamurti and Davis co-founded a startup company called Naima Health with their longtime collaborator, Hyagriv Simhan, professor of obstetrics, gynecology and reproductive science at the University of Pittsburgh. The combination of clinical expertise with Krishnamurti and Davis’ research forms a unique blend of perspectives to tackle women’s health disparities, and Naima Health has subsequently formed partnerships with UPMC Magee-Women’s Hospital and UPMC Enterprises to address these challenges.
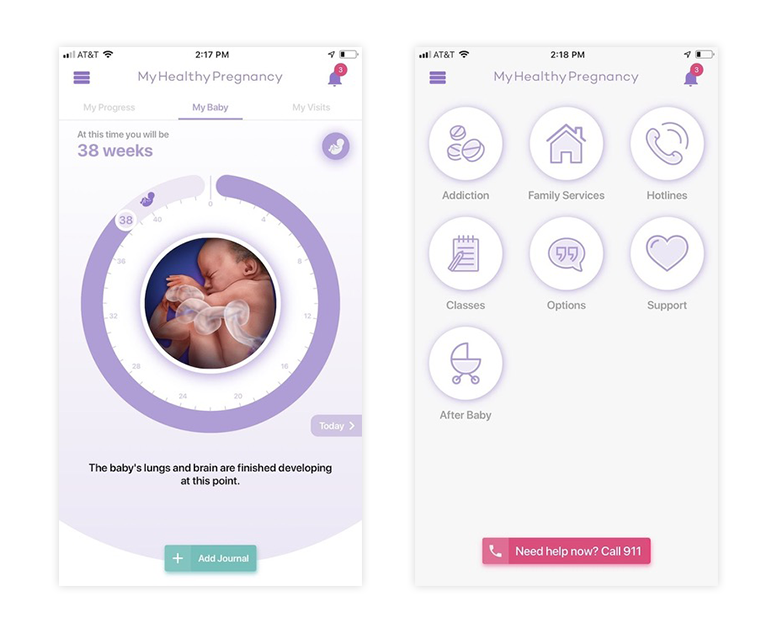
Naima designed an app called My Healthy Pregnancy (MHP) to benefit all pregnant patients, with a specific aim to improve outcomes for patients who are living in poverty or who are facing other complications.
“We thought an app might be a good, tangible way to communicate and get patients to disclose risk factors in ways they might not be able to in person,” Krishnamurti said.
Unlike most conventional pregnancy apps that compare the growing fetus to various forms of produce, MHP gathers risk data from users while communicating personalized health information about nutrition, weight gain or symptom assessment. Many of the app’s target users have knowledge gaps about appropriate diet or the dangers of smoking during pregnancy.
I think it’s totally interesting to know what vegetable your baby is sized like each week, but our goal is really to help deliver early intervention and offer support.
Tamar Krishnamurti, Assistant Research Professor, Engineering and Public Policy
MHP’s algorithm learns as each user provides information and determines what messaging is most beneficial for each individualized user. For instance, the app can prompt users to call their physician in response to abnormal bleeding.
Some, Krishnamurti found, are living in fear of their personal safety. One user confessed via the app that her partner “shot at me… because I used to date his cousin.” Those patients are the ones who keep Krishnamurti up at night.
“Thinking about intimate partner violence took a lot of work,” she said, noting that Naima worked very intentionally to refine the language the app uses as well as the information it records in the user-facing interface. “When you are in a violent situation, you are often being monitored by your partner,” she said. “It’s hard to make technology that someone else can’t access.”
If a patient discloses or if MHP detects the user is in danger of domestic violence, the app offers resources and prompts them to take action, like calling 911. MHP then removes traces of that correspondence after alerting the patient’s physician.
“We let users know from the beginning that someone might see the information if they choose to disclose it,” Krishnamurti said. “We encourage the patients to drive the disclosure process.”
Source: College of Engineering
After a pilot study at a high-risk pregnancy clinic for low-income patients, MHP showed promising results. Patients increased their stated intent to breastfeed, lowered levels of perceived stress, and had a safe mechanism for reporting intimate partner violence, depression and drug use.
Krishnamurti and Davis also noted that transportation to the clinic presented a barrier for the patients, so they partnered with Uber to offer test subjects a ride to prenatal appointments via the app. Attendance at clinic increased from 50% to 84%—89% among the highest risk pregnant patients.Naima Health is currently conducting beta testing of MHP at UPMC, so all obstetrical patients with a MyUPMC account are given access to the app as part of their prenatal care package.
Krishnamurti and Davis are looking to enter the postpartum space—where patients can experience fatal hemorrhage, dangerously high blood pressure, the onset of postpartum mood disorder, and any number of factors contributing to the rising rate of preventable deaths in the United States—as well. Naima Health is actively seeking funding to strategically expand their algorithm and the care they can provide through the app in that critical time period between delivery and the six-week postpartum checkup.
“We would love to do so much more,” Krishnamurti said.
