A breath of fresh perfluorocarbon
Inhaled drug delivery uses inhaled air to carry medication to disease-affected areas and alveoli of the lungs. However, many chronic diseases limit the ability of inhaled medications to reach the affected areas. Diane Nelson has been working on what she believes is the solution: liquid perfluorocarbon emulsions.
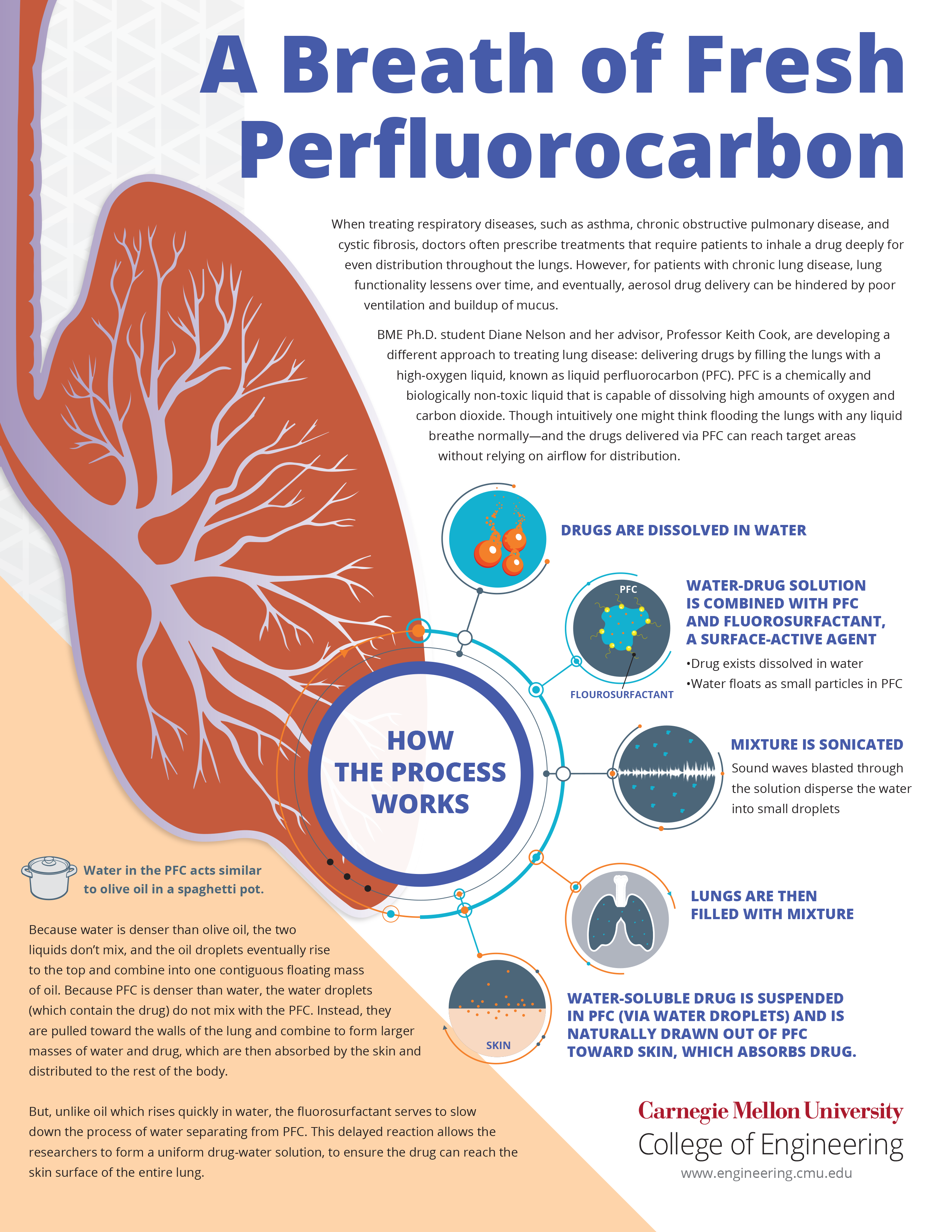
Inhaled drug delivery has long been held as the golden standard for treating conditions affecting the lungs, with inhaled air carrying medication to the affected areas and alveoli of the lungs. However, many diseases, such as chronic obstructive pulmonary disease (COPD) or cystic fibrosis (CF), cause inflammation or mucus buildup in the lungs, which limit the ability of inhaled medications to reach the affected areas. Diane Nelson, a biomedical engineering Ph.D. student in the lab of Professor Keith Cook, has been working on what she believes is the solution: liquid perfluorocarbon (PFC) emulsions.
If we can show that this delivery method is better than inhaled delivery, we’re hoping that for severe cases, this method will be better than mechanical ventilation.
Diane Nelson, Ph.D. student, Biomedical Engineering, Carnegie Mellon University
“Our proposed solution is to deliver drugs by filling their lungs with a liquid, and this will give you a uniform distribution of medication,” says Nelson. In other words, the PFC method of drug delivery—a method that washes a liquid solution containing suspended medication particles through the lung—holds the potential to revolutionize lung disease treatment.
For most people, the first thought that comes to mind when they hear the words “fluid-filled lungs” is obvious: drowning. However, PFCs have a high oxygen solubility, meaning that the liquid can be saturated with oxygen so that the body can continue respiration despite the lungs being completely filled with liquid. In fact, PFC liquids may actually help increase oxygen absorption by clearing out mucus blockages, and they have the added side effect of exhibiting anti-inflammatory qualities.
Source: Carnegie Mellon University College of Engineering
A closer look at the process of delivering drugs by filling the lungs with PFC
The biggest challenge posed by PFC drug delivery is not actually in the liquid nature of the PFCs, but in how they interact with other liquids; most medication delivered in liquid form must be soluble in water to create an aqueous solution. “Several people have been trying to deliver drugs using this method,” explains Nelson, “but the issue is that water and PFC don’t dissolve together. We need a uniform distribution, but if we put them together it would just be like water and oil: water at the bottom, oil at the top.”
That’s where Nelson’s research comes into play. Nelson is developing a method for delivering drugs using liquid PFCs, the topic of a CMUThink Webinar she presented on her work in October.
The first step is to dissolve the drugs in water. Then, these water-drug solutions are combined with the PFC and a fluorosurfactant, a surface-active agent. “Like I said, water and oil, but if you put a little soap in the middle it helps blend the two together.” The mixture is then sonicated, which means that sound waves blasted through the solution disperse the water into small droplets.
“The surfactant is like a soap,” explains Nelson. “It acts as a casing for the water and makes little droplets that spread evenly throughout the PFC.”
“So far, liquid ventilation itself has been performed clinically. That’s just putting PFC in patient’s lungs, no drugs added,” Nelson said, “If we can show that this delivery method is better than inhaled delivery, then we’re hoping that for severe cases, this will be better than mechanical ventilation where they just add antibiotics to the bloodstream instead of directly to the lungs.”
This method promises possible applications for a variety of cases if successful. For conditions like COPD, CF, and acute respiratory distress syndrome, PFC emulsions could prove an effective new way to eliminate inflammation and mucus during the drug delivery process, decreasing the risk of chronic infection while increasing the patient’s ability to breathe deeply. Liquid ventilation, minus the drugs, is already seeing use in neonatal units on premature infants with underdeveloped lungs. The method has even been considered as an alternative to intravenous (IV) drug delivery in some instances. Unlike IV delivery, drugs delivered through the lungs bypass the first pass through the liver, which can often filter much of the medication from the blood before it has a chance to reach the rest of the body.
In short, the possible benefits of Nelson’s work are as promising as they are varied. To leave you with the closing line of her winning presentation from CMU’s 2017 Three Minute Thesis competition, “Perfluorocarbon drug delivery is a great method to help patients breathe easier.”
